Welcome
Welcome to the Intensive Care Unit! We hope you enjoy this attachment and gain useful clinical experience. Assessment and management of the sick patient is a core part of practice as a junior doctor. We hope this attachment will give you some knowledge and strategies to take forward for your future career, wherever that may lie!
The intensive care unit (ICU) is situated on the 1st floor of the hospital, above the emergency department.
We very much hope that you enjoy your attachment, and that we hope to inspire you to join our ICU community in the future. Please contact me if you have any questions, or indeed suggestions for improvement of our teaching programme.
Key Contacts
- Undergraduate Lead – Dr Fiona McIlveney
Overview
We are referred adult patients from any specialty within the hospital who require some form of critical care intervention or enhanced monitoring. The ICU has 19 beds, of which 2 may be used by cardiology for enhanced monitoring and intervention.
We admit an average of 400 patients to the ICU and ~1000 to HDU. These admissions are now amalgamated into our one ICU, so you should have the opportunity to gain a reasonable amount of experience during your time with us. As soon as you arrive, we will help to familiarise you with where the safety equipment is kept on the unit, and our day to day practices.
For day to day activities see ICU/Anaesthetics junior doctor induction page.
This document will also give information about the different types of interventions made at each ‘level of care’.
Staffing
During each shift, a senior nurse is responsible for the day to day clinical running of one side of the unit together with the consultant intensivist. Patients are nursed on a 1:1 or 1:2 nurse:patient ratio depending on their level of dependency. The nursing staff vary in experience but are happy to support and help you during your attachment. Feel free to ask if you have any questions for them.
There are a variety of junior doctors who work in ICU at any one time. They include foundation year doctors, trainee anaesthetists at various stages, and occasionally doctors from other specialties such as emergency medicine, general medicine and ageing and health.
The unit is covered by two consultants each day, one for each side. Should you have any clinical questions/concerns regarding a patient, you can approach either for assistance. Either consultant may take referrals for new patients depending on workload.
Confidentiality
In the past trainees have printed out a list of the patients we have on the ward, which they have then carried around in their pockets. Inevitably, these lists have fallen out of a pocket whilst in a hospital corridor. It is preferable that patient lists are not printed out at all, but if this must happen then under no circumstances must they be taken off the ward. We cannot overemphasise the seriousness, with which the hospital management would regard such breaches of patient confidentiality.
Miscellaneous handy hints
Where possible, we have tried to come up with guidelines/protocols to assist you in your day to day work. Many of these can be found at the main desk; on the main computer; or at each bed space. They include such things as:
- An antimicrobial guideline for a variety of infective situations
- A ventilatory weaning guideline is available and all patients on a ventilator should have a weaning plan each day (even if it is to state that no weaning should take place that day)
- Emergency management of airway difficulties, including tracheostomy guidance is found at every bed space. Alert staff with airway skills early if you believe there is a potential airway problem.
You may be interested to peruse these during your attachment.
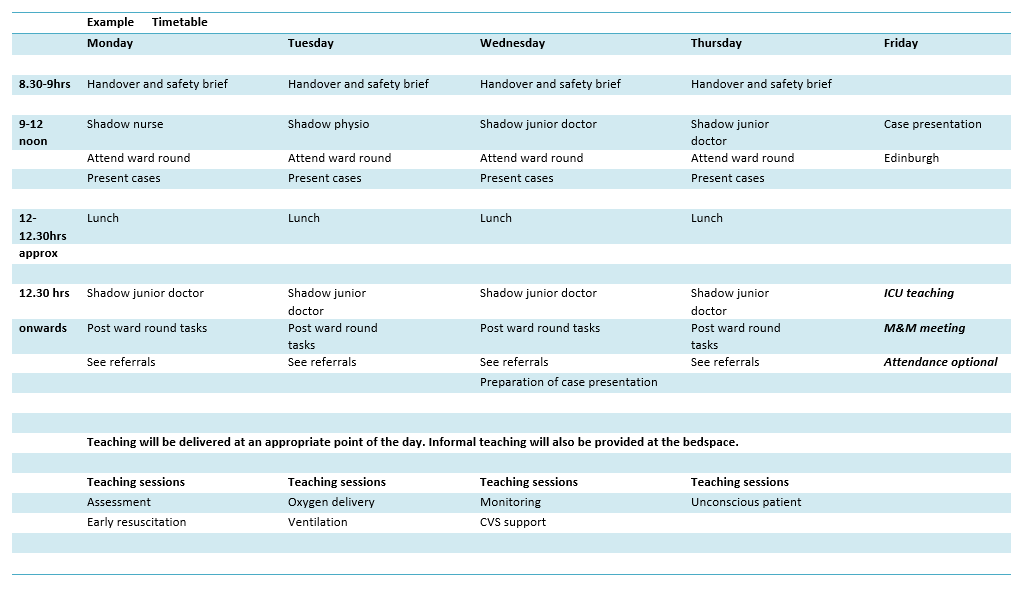
Tutorials
Each day there will/should be plenty of informal teaching during the ward round/discussion of cases/practical skills etc. There is also a plan for more formal tutorials to cover the educational objectives of your rotation. These are included in your rota template. The timing of these is suggested, and may be impacted by unexpected clinical activity but we would aim to deliver them at some point during your week.
In addition, there are excellent teaching modules on Scottish Intensive Care Society website, which you should go through and you will receive a certificate for your educational portfolios as a result of this. The modules cover a wide range of important topics:
Weekly morbidity and mortality meetings occur on a Friday afternoon. These are intended as a multidisciplinary meeting to improve our management of patients with critical illness and aid our learning and should occur in a safe and supportive learning environment. Every death will be discussed and learning points recorded, subsequently these will be discussed at an anaesthetic lunchtime meeting with the whole department. Your attendance at this is not compulsory, but you are very welcome to attend if you wish and have no other educational commitments.
Assessment/Case presentation
These occur at the end of your ICU week, due to current circumstances these will take place on line. Your university will provide details.
Each student gives a ten minute presentation based on the patient they have chosen during the week, followed by a short discussion. A powerpoint presentation is most popular, but choose whatever medium you are most comfortable with. A maximum of 10 slides, with no more that 6 bullets points per slide should be achieved.
Give a brief history of the patient presentation and management. Consider:
- How did the patient present?
- What demonstrated deterioration of this patient?
- How were they managed then?
- What was the cause of the deterioration / illness?
- What are the learning points from this patient?
Try to maintain an overview of events, and avoid unnecessary details. Remember to bring your presentation and a paper copy in case of IT failure to the presentation session.